Mold Protocol for Children with ASD and PANS
How to use itraconazole and other agents to treat mold-related illness in children and aults.
Disclaimer:
The information in this post is intended for use by healthcare professionals. By accessing this document, you acknowledge that you are a pediatric healthcare practitioner authorized to provide care to children, and agree that the contents of this document and any materials and programs provided by Dr. Pejman Katiraei, DO through his websites and social media accounts, are for informational purposes only and are not intended to provide medical advice, diagnose, or treat any health condition.
It is your responsibility to ensure the safety of any medication or nutritional, herbal, or homeopathic supplements, or any treatment plans that you develop for your patient. The use of any information provided by Dr. Pejman Katiraei in this document or other materials is solely at your own risk. You agree to hold Dr. Pejman Katiraei and Wholistic Kids and Families and Wholistic Minds harmless for the decisions you make for your child or patient. Information provided or referenced in this document and used by you DOES NOT create a doctor-patient relationship between you, or your patients, and Dr. Pejman Katiraei.
Information and statements regarding dietary supplements have not been evaluated by the Food and Drug Administration and are not intended to diagnose, treat, cure, or prevent any disease.
THE PROTOCOL
CLINICAL PRESENTATION AND HISTORY
1) Clinical History - The possibility of mold-related disease needs to be first assessed through history. Mold exposure can cause a wide range of clinical findings. While no individual finding is definitive for mold exposure, children who are exposed to mold typically present with a clustering of signs and symptoms across different systems. The larger the number of findings, the higher the likelihood of mold-related illness.
a. Other considerations:
i. If the child has siblings, you may find some of these signs/symptoms in them.
ii. Some children are born in damp environments, whereas others are exposed later. These later cases tend to have unremarkable PMHx, with “sudden” development of physical and mental health challenges within 6 months of moving or other change in environment (classroom/daycare/gym).
iii. If the exposure is within the home, typically one parent presents with fatigue, brain fog, etc. – see below.
2) Signs and Symptoms of Possible Mold Exposure (Bolded findings are more indicative of mold exposure)
a. Early childhood (only if child was born in damp home):
i. Significant colic (>2-3 hours fussiness requiring significant intervention to calm them) typically lasting >3 months of age
ii. Significant reflux lasting >6 months of age
iii. Atopy (eczema, allergies) < 1 year of age
iv. Food allergies or sensitivities in 1st two years of life.
v. Low tone with delayed gross motor skills (crawling 8-9 months, walking 14-15 months..)
vi. Delayed expressive language.
vii. Vaccine-related injury.
b. General
i. Low vitality - tired regularly despite a good night’s rest
ii. Low endurance/stamina - tires easily with prolonged/high activity, or will run but then crashes and takes a while to recover
iii. Muscle fatigue - will have muscle pain with exertion
iv. Low tone
v. Poor weight gain – dropped more than 20% on weight graph or has failure to thrive (<5% weight on chart)
vi. Poor growth – dropped height percentiles or failure to thrive (<5% height on chart)
vii. Low appetite – prefers to graze and may only eat 1-2 meals per day
viii. Very picky eater – prefers carbs and soft textures like chicken nuggets
c. Gastrointestinal
i. Multiple food intolerances or allergies
ii. Tendency for constipation or diarrhea
iii. Red ring around anus
iv. Unexplained abdominal pain
v. Multiple cavities
vi. Elevated SIGA or calprotectin on stool testing
vii. Elevated candida on OAT or stool testing
d. ENT
i. Moderate to persistent mouth breathing
ii. Significant congestion/allergies
iii. Enlarge adenoids or tonsils
iv. Snoring or disrupted breathing while sleep
v. Prolonged congestion after a viral infection
vi. Recurrent ear infections – possibly needing PE tubes
e. Pulmonary:
i. Recurrent “croup” or other severe respiratory infections
ii. Asthma with severe viral-induced airway inflammation/restriction
f. Sleep
i. Poor sleeper (“colicky,” “never a good sleeper”)
ii. Takes 45-60+ minutes to fall asleep despite no media before bed/good sleep hygiene
iii. Wakes up in the middle of the night, typically 2-4 AM, and has a hard time falling back asleep
g. Derm
i. Gets rashes that come and go, or from being touched/held (+dermatographia)
ii. Rashes triggered by warm showers or hot water
iii. Intense swelling to insect bites
iv. Moderate to severe eczema, including significant itching
v. Very thin and slow-growing hair
h. Neurological:
i. Sensory findings (auditory, tactile, olfactory, vestibular) that can impact sociability
ii. Poor motor planning
iii. Tics or seizure-like episodes
iv. Abnormal/irrational fear response or anger/aggression (anger is rooted in fear)
v. Significant anxiety, including separation anxiety
vi. Learning disabilities
1. High distractibility or impulsivity
2. Struggles to learn/retain math concepts (working memory)
3. Various processing errors
4. Poor memory or executive functioning
5. Visual processing
a. Skips lines when reading or has much greater difficulty with reading vs other subjects
b. Has poor hand-eye coordination
c. Toe-walks
3) Family History
a. The above findings may be present in the siblings of this patient if exposure is at home during a time that the sibling was living in that home as well.
b. Adults (these findings can be in parent OR teacher – depending on where the contamination is)
i. Moderate – severe fatigue (“I feel tired all the time, but I thought this was just because of…”)
ii. Brain fog or changes in memory
iii. Chronic congestion/allergies
iv. Adult asthma
v. Eczema or psoriasis (new onset or getting progressively worse)
vi. Arthritis, thyroiditis, or other autoimmunity
vii. Myalgias
4) Conventional Lab findings:
a. Marginal liver enzyme elevations (usually AST >30 U/L, but can be both AST/ALT)
b. Low white blood cell count (3,500 – 4,000)
a. Low absolute neutrophil count (800 – 1,400)
b. Low RBC Zinc
c. Low iron
d. Multiple food allergies on IGE testing
e. Thyroid antibodies
f. Positive ANA (>1:80 present in approximately 50% of children exposed to mold)
DIAGNOSTIC TESTING
1) Organic acids
a. Clinical accuracy: The fungal markers on Genova or Mosaic organic acids have a false negative rate of >50%. As such, this test must never be used as a single diagnostic tool for assessing mold exposure.
b. Fungal markers: Even marginal elevations in fungal markers, especially tartaric acid can be indicative of current or past mold exposure.
c. Oxalates: Per research from Dr. William Shaw, Candida and Aspergillus are capable of producing oxalates. While spinach, rhubarb, and almonds are some sources of oxalates, spikes in oxalates can also be indicative of fungal dysbiosis, which can easily occur due to mold exposure.
d. Metabolic markers: Mold exposure causes a spike in mycotoxins and appears to cause endotoxemia. Both mycotoxins and endotoxins are capable of disrupting mitochondrial function and fatty acid oxidation. While numerous other toxins are also as capable, metabolic markers in combination with noted clinical findings and other lab findings may be suggestive of mold-related disease.
2) Urine mycotoxin testing
a. Clinical accuracy: Urine mycotoxin testing was originally developed to assess mycotoxin exposure from DIETARY sources, and thus these tests can demonstrate high-level exposure that is dietary (grains, milk, nuts, etc.). I have also found that children who are toxic appear to lose the ability to secrete the mycotoxins into their urine. These tests appear to have a 30-50% false negatives rate in children impacted by mold (depending on numerous factors).
3) Antibody testing
a. Individuals who are exposed to water-damaged buildings have elevated antibodies against mold and mold toxins, as demonstrated in a 2003 paper by Vojdani and colleagues. The validity of this study has been called into question. In my experience in testing hundreds of children impacted by mold, antibody testing is by far the most reliable way to assess exposure. The testing appears to have a false negative rate of approximately 20%, with a high specificity.
b. Reliable companies:
i. Alletess has a basic mold panel that is $200 and checks for IGE, IGG, and IGA antibodies against the molds. Typically, an IGG antibody level of >30mg/L is suggestive of past OR current exposure. IGG antibodies can be elevated for years after exposure and thus cannot indicate the time of exposure. IGA antibodies may be suggestive of colonization.
ii. Mymycolab holds the patent for antibody testing against mold toxins, and this testing does offer superior specificity. The test is approximately $400 and may have slightly less sensitivity in younger children.
iii. Other labs: What about Quest or LC? While IGG testing for molds is available through these commercial labs, it is rarely covered by insurance, and I have questioned their reliability. I do not have experience with IGG mold testing through Real Time Labs to comment.
4) Other labs
a. General: All children who may be exposed to mold should have basic lab testing: CBC with diff, CMP, TSH, and Free T4.
b. ANA: approximately 30% of mold-impacted children have an ANA of 1:80. Another 10-20% have an ANA of 1:160 or higher, and these levels could suggest gut disruption.
c. Thyroid peroxidase antibodies: 10-20% of children impacted by mold have some elevation of thyroid antibodies, and of these children, approximately 20% have frank Hashimoto’s.
d. Iron studies and RBC Zinc: Mold toxins have been demonstrated in animal studies to disrupt the absorption of iron and zinc. In my experience 40-50% of mold-impacted children have some degree of iron deficiency, and of this 10-20% with severe deficiency. Zinc deficiency is present in 60-70%, with 20+% presenting with severe zinc deficiency.
e. Gliadin IGG and IGA: There is immune cross-reactivity between Candida and gliadin. Outside of ruling out frank Celiac Disease, when marginally elevated, gliadin antibodies may suggest fungal dysbiosis, which can be a result of mold exposure.
f. Saccharomyces cerevisiae IGG and IGA (ASCA): Mycotoxins are extremely capable of disrupting tight junctions and inducing gastrointestinal inflammation. While frank inflammatory bowel disease is only found <5% in mold-impacted children (higher than in general population), approximately 70-80% of these children do have mild elevation of these antibodies. These findings appear to not only suggest a compromise of the gut barrier, but perhaps may also indicate fungal dysbiosis since Candida is an immunogen for ASCA.
g. Matrix metalloproteinase-9: MMPs are enzymes that are responsible for wound healing and tissue repair. When elevated, they suggest damage or compromise of the tissue matrix, especially within the gut. Dr. Ritchie Shoemaker first found that MMP-9 can serve as a useful and highly sensitive biomarker of mold-related disease (sensitivity >90%), despite the low specificity. Despite the laboratory reference ranges, per Dr. Shoemaker a normal range of MMP-9 is 85-332 ng/mL. MMP-9 up to 550 suggest some degree of tissue disruption/repair that is manageable. The higher the MMP-9 level above 600, the more suggestive it is of tissue damage, and the higher the likelihood that the child’s immune system will be highly sensitive and unpredictable (especially if there are high levels of ANA and/or ASCA). Proceed with caution in these children.
5) Stool testing: Children with ASD should be tested for parasitic infections through companies with a high sensitivity. Companies like Diagnostic Solutions often give unreliable results. One reliable company is:
https://parawellnessresearch.com/
EVALUATING THE HOME/ENVIRONMENT
1) Background: If mold exposure is suspected as a contributing factor to a child’s ASD presentation, it is critical to understand their exposure. As noted, exposure can occur at any time, anywhere.
2) Differentiating based on history
a. Children born into a home with mold: As noted above, these children tend to present with abnormal clinical findings in infancy, including colic, reflux, atopy, food intolerances, failure to thrive, recurrent otitis or pulmonary disease, etc.
i. It is important to realize that 1-2 years of significant exposure in the first few years of life is sufficient for chronic changes to the immune system and gastrointestinal tract, thus allowing for persistent ASD symptoms despite removal from the environment.
b. Children exposed in later years: Often these children have an unremarkable past medical history, only to “suddenly” experience cognitive/developmental regression within 6 months of moving into a new home.
c. Exposures outside of the home: Approximately 20% of all schools in the US have been found to have mold. If a classroom has mold usually there are multiple children with significant clinical findings as noted above. The teacher(s) may experience health challenges as noted for the adults. Exposures can also occur in daycares or the homes of relatives (grandparents).
3) Testing
a. Conventional environmental testing is HIGHLY problematic and unreliable. Families commonly state, “We had our home tested and there is no mold.” These statements can be misleading because of the problematic testing data the family previously received. Click here for a detailed discussion about the limitations of environmental testing.
b. The most accurate/sensitive screening tool to assess an environment is quantitative PCR analysis of the dust from within the indoor space. The ERMI was created by the EPA as a research tool to help assess space for mold contamination. While the ERMI score is inherently problematic, other companies have taken this technology and improved its reliability. Currently, the best test on the market is:
https://www.thedusttest.com/
. The results from this test are reviewed by a qualified professional and homes are given a “code.”
i. Sampling: The Dust Test comes with its own instructions. I advise all families to thoroughly clean/dust the home, then to allow dust to settle for ideally two weeks before collecting the specimen. Accuracy is dependent on adequate dust collection. Sample all areas that the child spends time in.
ii. Understanding the Dust Test:
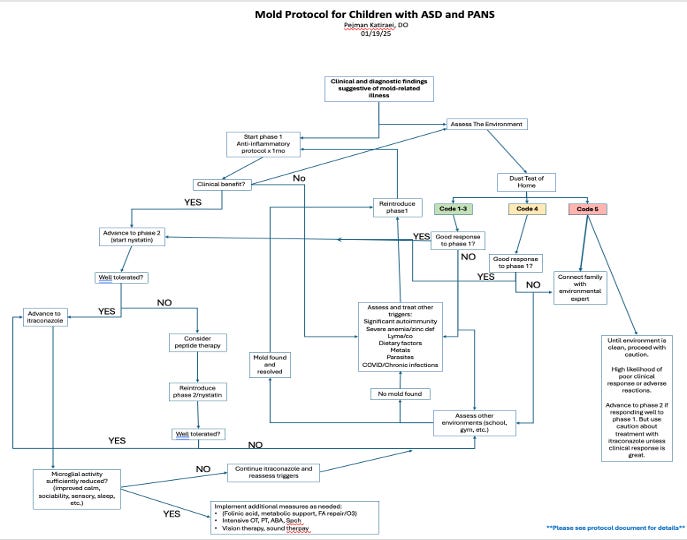
1. Codes 1-3 are suggestive of a clean home. If the child is presenting with concerning symptoms and not responding to treatment protocol AND Dust Test is a Code 1-3, inquire about other environments that the child may be in, such as their school. Sampling errors can impact accuracy of this test. If any question, consult with an indoor professional (see below).
2. Code 4 is a yellow flag – may suggest contamination. A child living in a code 4 home may still respond well to treatment.
3. Code 5 is a red flag – may suggest there is sufficient/significant contamination where a child’s clinical progress may be limited. If the child has limited clinical progress or reacts to multiple treatments, the child’s environment should be first cleaned/controlled before proceeding.
iii. Next steps: The Dust Test is only a screening tool and requires in-person testing by a qualified indoor professional for confirmation of contamination. The Dust Test company offers consultants who can do in-person testing as needed. A large list of other professionals can be found here: https://iseai.org/iep-list/ It is important to advise the family against hiring random inspectors, as they regularly miss subtle, yet clinically-important levels of contamination and mold.
4) Controlling the environment: For a detailed discussion on how to help a client control/limit exposure, please see this video:
TREATMENT
1) Diet: Outside of reducing/eliminating gluten and dairy from the diet of these children, it is also useful to consider the following:
a. Simple carbs and sugar: Can cause a reflexive hypoglycemia and contribute to worsening fungal dysbiosis.
b. High-histamine foods: Some high-histamine foods are considered healthy foods, including bone broth and fermented foods. Given the picky nature of many children with ASD, processed meats should also be considered. Children with fungal dysbiosis have DAO enzyme deficiencies and thus struggle to break down histamine, and excess histamine in the diet may exacerbate a catecholamine effect within the CNS. High Histamine Foods:
a. Food colorings and preservatives (trigger significant mast cell activation)
b. Fermented or pickled foods: Sauerkraut, kimchi, kombucha (high in histamines)
c. Bone broth (very high in histamines)
d. Dried fruits
e. Most cheeses
f. Avocados
g. Processed meats (hot dogs, salami, smoked meats, fermented ham and sausage…)
h. For a detailed listing: https://www.histaminintoleranz.ch/downloads/SIGHI-Leaflet_HistamineEliminationDiet.pdf
2) Phase 1: Reduce inflammation
a. Unless existing supplements were clearly found to be making a difference, please consider discontinuing all other supplements during this phase. Mold-impacted children have extremely sensitive gastrointestinal immune responses that may react to just about anything including: citric acid, probiotics, fish oils, flavorings, additives, natural food coloring, etc.
b. Basic anti-inflammatory protocol – administer for 4-6 weeks and monitor clinical response:
· Administration: The below products can be mixed into any cold/room temperature food or drink. Some examples include: apple sauce, favorite juice (ideally thicker like orange juice), or even vegan pudding…
· Mirica (Palmitoylethanolamide + Luteolin)
1. Risk: Children with highly unstable immune responses (5-10%) may react
2. Dosing: 3-6 y/o 1 per day, 6-12 y/o 2 per day, 12+ 2-4 per day
3. Mechanism:
a. Palmitoylethanolamide – reduces microglial and mast cell activation
b. Luteolin – reduces microglial AND mast cell activation
· Histamine Digest (DAO Enzyme)
1. Risk: Children with ++ adrenal/HPA imbalance may react (10% - especially those with high metabolic errors). If this occurs, consider carnitine, as mitochondrial function drives steroidogenesis.
2. Dosing: 3-6 y/o ½ - 1 per day, 6-12 y/o one capsule 1-2 times a day, 12+ 2-4 per day
3. Mechanism: Breaks down histamine within the gut (systemic histamine levels)
4. Sourcing:
a. Animal-derived: Seeking Health Histamine Digest - https://www.seekinghealth.com/products/histamine-digest-formerly-histamine-block
b. Vegan: NaturDAO - https://www.naturitas.us/b/naturdao - difficult to source. Comes from Spain.
c. Opening of capsules – despite the manufacturer’s warnings, all DAO enzyme capsules can be opened and mixed into cold food or drink without loss of efficacy. NaturDAO tablets should not be crushed.
· If a child is very sensitive, start at 50% for both supplements and build up over 1-2 weeks.
c. Additional supplements (please make sure to use supplements free of citric acid)
· Vitamin D/K2
1. Suggested dosing: 3-6 y/o – 500 – 1,000IU/day, 6-12 y/o – 1-2,000IU/day
2. Possible source: https://www.pureformulas.com/product/vitamin-d-k2-liquid-by-thorne/1000011127
· Zinc
1. Suggested dosing: 3-6 y/o – 4-10mg/day, 6-12 y/o – 6- 10+mg/day
2. Possible source: https://www.pureformulas.com/zinc-liquid-drops-15-mg-388-fl-oz-115-ml-by-dr-mercola.html
· Carnitine
1. Errors in fatty acid oxidation are the most common form of metabolic errors in mold-impacted children. Metabolic support can help optimize adrenal function (and a host of other physiological processes), and thus further stabilize the system. Carnitine is the only metabolic support that is suggested at this time since other mito/metabolic supplements/treatments may exacerbate CNS findings at this stage.
2. Suggested dosing: 3-6 y/o – 500mg/day, 6-12 y/o – 500 – 1,0000mg/day
d. What to look for: Intentionally, no sedating or anxiolytic products or compounds are used at this stage to allow the treatments to also serve as a semi-diagnostic tool. If a 20-30+% reduction in anger/aggression, anxiety, sensory findings, etc., are found, this can suggest that the symptoms were inflammatory in nature and provides soft evidence that future treatments will likely be helpful.
3) Phase 2: introduce after 1-2 months
a. Additional calming agents
· Lithium
1. Lithium not only potentiates GABA receptors but also acts as a CNS anti-oxidant. Humans primarily obtain lithium from drinking water. Reverse osmosis water strips all minerals out of the water, and thus lithium deficiency is more common in those who drink RO water. Treatment is to simply restore nutritional levels.
2. Dosing (for all ages) – Loading dose for one week 4-5mg per day. If benefit is found, continue with 4-5mg 2-3 times a week
a. https://www.iherb.com/pr/kal-lithium-orotate-drops-lemon-lime-2-fl-oz-59-ml/78420
b. https://www.iherb.com/pr/brainmd-lithium-orotate-5-mg-60-vegan-capsules/135086
· Magnesium Threonate
1. Magnesium threonate is most effectively absorbed into the CNS and can help calm the nervous system.
2. Suggested dosing – based on elemental magnesium - 3-6 y/o – ½ capsule (70-144mg)/day, 6-12 y/o – 1-2 capsules/day
b. Nystatin and gastrointestinal fungal dysbiosis
· Background: Mycotoxins can directly trigger CNS inflammation/microglial activation through intranasal absorption, but the more serious and chronic effects occur through the direct and indirect disruption of gut permeability and the mycobiome. Fungal dysbiosis of any kind can trigger rather significant levels of inflammation both within the gut and CNS. Any sudden change to the mycobiome can exacerbate CNS/ASD findings, and thus it is critical that the rebalancing of the microbiome be done slowly at a pace that is tolerated by the child. Because nystatin has a limited antimicrobial effect directed at Candida, it is a desirable first-line treatment for fungal dysbiosis. Only 30-40% of children will have clinical improvements with nystatin (CNS or gut). The main purpose of nystatin is to ensure that the child’s gut-immune response is stable and ready for future treatments.
· Nystatin ordering:
1. Regular liquid nystatin has a host of inactive ingredients that can be highly problematic to a sensitized gut: Inactive ingredients: alcohol (≤ 1% v/v), artificial wild cherry flavor, banana flavor, D&C yellow #10, FD&C red #40, glycerin, USP, magnesium aluminum silicate, methylparaben, NF, potassium phosphate dibasic, USP, propylene glycol, USP, propylparaben, NF, purified water, USP and sucrose 33.5%. May also contain citric acid, USP for pH adjustment.
2. As such, it is always ideal to have nystatin compounded through a local compounding pharmacy with minimal preservatives. Possible RX: “5ml qday - 100,000IU/ML nystatin liquid compounded without colorings and minimal preservative in suspension form for a 30-day supply.”
3. Dosing: Follow general prescription guidelines for age. Once a day dosing is sufficient. Start at 2 ml per day and build to 5 ml qday over 2 weeks. If the family sees increased anxiety, sensory findings, insomnia, or other adverse effects, they are to stop for 5 days and resume at 50% dose.
c. Serum Bovine Immunoglobulins (SBIs)
· SBIs are purified immunoglobulins that can be extremely useful in optimizing gastrointestinal function by:
1. Improving gut inflammation and barrier (increase tight junctions)
2. Binding microbial antigens, preventing their translocation
3. Improving beneficial bacteria and systemic inflammation
· If a child is tolerating nystatin well, SBIs can be a useful addition to enhance gut function.
· Dosing (1 scoop = 4 capsules)
1. 3-6 y/o – ¼ - ½ scoop (500-1,000mg), 6-12 y/o – ½ - 1 scoop
· Sourcing – two well-regarded products are SBI Protect and Mega IGG 2000. Both come in powders and capsules, and are nearly the same concentration.
4) Phase 3
a. Itraconazole
· Mechanism: Itraconazole is a broad-spectrum antifungal with antimicrobial effects against Aspergillus and other molds that may colonize the body. What is less recognized are all the other properties Itraconazole has. It has gut and central immune-modulating properties. I strongly suspect itraconazole is a potent inhibitor of the microglia and produces many of the clinical benefits not just by improving the mycobiome, but by modulating the immune response at multiple levels. As such, it is important to consider this medication as an immune modulator and antifungal.
· Dosing: 5mg/kg with a max of 100mg/day for older children.
· Suggested use: “If your child is tolerating daily doses of nystatin for 4 weeks, then start itraconazole. Only advance/increase frequency if your child is doing well. If your child appears tired, or sleepy, stop the medication and let your provider know.”
1. Weeks 1-2: One dose every 3-4 days.
2. Afterward: Increase to every other day dosing.
** Some use daily or even higher doses of itraconazole. I have not found this to be clinically superior to every other day dosing, as long as the other noted factors are taken into account.
· Testing: It is advisable to check liver enzymes 6-8 weeks after starting, and ideally every 2-3 months thereafter. It is generally well tolerated. Children with elevations with LFTs typically present with fatigue or looking unwell (<5% of all cases).
· Duration: If the child is tolerating itraconazole well, the greatest efficacy is found after 4-6+ months of continuous treatment.
5) Next steps
a. I have found that once the inflammatory response and gut permeability are controlled, mitochondrial support, methylation, fatty acid replacement, and other such treatments are far more easily tolerated and efficacious. This increased efficacy also extends to ABA therapy, OT, Speech, etc., since the children are often much more calm and receptive to the therapy. These interventions can be started in the middle of the itraconazole course or once the child more calm and regulated (sometime happens even after start of nystatin).
b. Indicator of clinical success: Successful treatment should result in a significant reduction in microglial and mast cell reactivity. Clinically this should present as improvements in:
· Sensory findings/distortions (auditory, tactile)
· Anxiety (including social anxiety) and exaggerated fear response
· Aggression and irritability
· Sociability including possible signs of improved oxytocin and serotonin function
· Sleep (falling and staying asleep)
· Digestion (constipation/diarrhea OR improvements in food sensitivities)
· Slight improvements in food aversions (willing to try/take a few bites of new foods)
c. After 4-6 months of itraconazole, if the child is doing well, one can stop the medication and monitor. It is important to advise the family that the anti-inflammatory effects wear off over 3-4 weeks, and they must carefully observe to make sure the child does not regress during this time. If regression is noted, itraconazole can be resumed.


I like Pure Encapsulations. I honestly have no idea where they source their carnitine from. Dr. K
What is source of Carnitine??